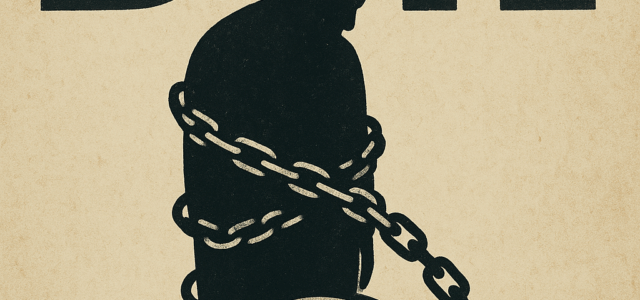
Why We Hate the BMI: The Tyranny of a Two-Dimensional Metric
The Body Mass Index (BMI), calculated simply as mass divided by the square of height (weight/height2), is arguably the most common and despised metric in modern medicine. While its simplicity made it a statistical godsend for large-scale population studies in the 20th century, its continued use as a definitive measure of individual health is an obsolete practice that invites criticism, misdiagnosis, and significant personal distress. Our hatred for the BMI stems from its fundamental inability to capture the three-dimensional, complex reality of the human body.
The Fault of the Fit and the Free Pass to the Frail
The most glaring indictment of the BMI is its indifference to body composition. It treats a pound of muscle identically to a pound of fat, which is where the measurement loses all credibility for a significant portion of the population.
- The Athletic Misclassification: Highly muscular individuals, such as powerlifters, rugby players, or sprinters, possess high bone density and large amounts of lean muscle mass. Because muscle is denser than fat, their weight often pushes them into the “overweight” or even “obese” categories. The BMI, in these cases, falsely labels an elite athlete at peak health as metabolically high-risk.
- The “TOFI” Trap: Conversely, the BMI can be dangerously reassuring for the “Thin Outside, Fat Inside” (TOFI) individual. Someone with a low amount of muscle mass, yet who carries excessive visceral fat around their organs, can still register a “normal” BMI. This score provides a lethal false-negative, masking a high risk for conditions like insulin resistance and Type 2 diabetes. The BMI is blind to this critical internal danger.
Ignoring Location: The Visceral vs. Subcutaneous Divide
In health, geography matters. A person’s metabolic risk is primarily determined by where their body fat is stored, a nuance the BMI entirely misses.
- The Threat of Visceral Fat: Deep abdominal fat (visceral fat) is an endocrine organ that actively secretes inflammatory hormones, directly contributing to heart disease, stroke, and systemic inflammation. This is the truly dangerous fat.
- The Passivity of Peripheral Fat: Fat stored in the hips, thighs, and buttocks (subcutaneous or gluteofemoral fat), typical of the “pear” body shape, is metabolically less harmful and can even be protective in some cases.
The BMI, by only considering total mass, sees no difference between a healthy “pear-shaped” individual and an unhealthy “apple-shaped” individual with a gut full of visceral fat, rendering it useless for assessing individual cardiometabolic risk.
A Historically Biased and Outdated Formula
The BMI’s origins are not rooted in medical science but in 19th-century statistics. It was created by Adolphe Quetelet, a Belgian mathematician, to study the “average man” of his time (European, male) for population censuses, not for clinical diagnosis.
- Racial and Ethnic Bias: Using a single formula globally ignores known biological and metabolic differences. For example, many Asian populations show increased health risks at lower BMI thresholds compared to European populations. A one-size-fits-all metric is inherently inaccurate when applied to global human diversity.
- The Height Distortion: The formula uses the square of height (height2). Mathematically, volume (and mass) scales closer to the cube of height (height3). This flawed scaling systematically inflates the BMI of very tall people and underestimates the BMI of very short people, adding a layer of calculation error that has nothing to do with health.
The Stigma and the Gatekeeping
Beyond its scientific flaws, the use of the BMI in clinical settings and institutional policy is a source of intense frustration and resentment.
- Medical Stigma: Physicians often rely too heavily on an elevated BMI, leading to a phenomenon known as “weight bias.” They may dismiss a patient’s actual symptoms (e.g., joint pain, fatigue) with the simple prescription to “lose weight,” delaying critical diagnosis and treatment for unrelated conditions.
- Barrier to Care: Insurance companies and medical systems frequently use BMI as a rigid cutoff for eligibility for certain procedures (such as fertility treatments or some surgeries), effectively penalizing individuals whose weight is high but whose metabolic health markers (blood pressure, cholesterol) are perfectly normal.
In conclusion, the BMI is not a measure of health; it is a cheap, two-dimensional screening tool from the 1800s. We hate it because it mislabels the fit, endangers the frail, perpetuates systemic bias, and serves as a blunt instrument of judgment that fails to respect the intricate, unique biological reality of the individual. For personalized healthcare, the tyrannical reign of the BMI must end, replaced by comprehensive, modern metrics that measure what truly matters.